How to Tell If You Have a Cavity: Expert Guide
How to Tell If You Have a Cavity: Expert Guide
Your tooth starts throbbing during lunch. You run your tongue across your back molars and feel something… off. Maybe a small pit or a tender spot that wasn’t there last week. The question hits you immediately: Do I have a cavity?
Dental cavities are one of those health issues that sneak up on you. They don’t announce themselves with fanfare—they whisper warnings that most of us miss until we’re sitting in the dentist’s chair. The good news? You don’t need to wait for professional confirmation to suspect you might have a problem. Learning to recognize the early signs of tooth decay can save you time, money, and a whole lot of discomfort.
This guide walks you through the telltale indicators of cavities, from the obvious to the subtle. We’ll cover what happens inside your tooth, how to spot trouble before it becomes expensive trouble, and when you absolutely need to call your dentist. Think of it as your personal cavity detection toolkit.
Common Signs and Symptoms of Cavities
The journey of a cavity typically begins silently. Tooth decay doesn’t hurt until it reaches deeper layers of your tooth structure. Early detection relies on noticing subtle changes rather than dramatic pain signals. Here are the primary warning signs that something’s brewing beneath the surface:
Tooth sensitivity ranks as one of the earliest red flags. You might notice discomfort when consuming hot coffee, cold ice cream, or sugary snacks. This sensitivity differs from typical temperature sensitivity because it’s localized to one specific tooth rather than a general pattern across your mouth.
Discomfort when chewing is another common indicator. If you find yourself avoiding one side of your mouth or noticing sharp sensations when biting down on particular teeth, a cavity could be the culprit. The pressure from chewing can irritate the decay and trigger pain signals.
Spontaneous pain without any trigger is often a sign that decay has progressed deeper into your tooth. This throbbing or aching sensation might come and go, but its presence suggests you need professional attention soon.
Bad breath and an unpleasant taste in your mouth can also indicate cavities. Bacteria colonizing the decayed area produce sulfur compounds that create these unpleasant odors and flavors. If your morning breath has become particularly offensive or you notice a persistent taste you can’t brush away, it’s worth investigating.

Visual Indicators You Can See
Sometimes cavities reveal themselves visually before they cause pain. Grab a mirror, good lighting, and take a close look at your teeth. Here’s what to watch for:
Discoloration and dark spots are perhaps the most obvious visual sign. Cavities typically appear as brown, black, or dark gray spots on the tooth surface. Early-stage cavities might look like subtle discoloration, while advanced decay creates obvious dark pits. The color occurs because bacteria and decay products stain the affected area.
Visible pits or holes indicate that decay has progressed significantly. If you can actually see a depression or small hole in your tooth, professional treatment is urgent. This stage means the decay has eaten through the enamel and into the dentin layer beneath.
Rough or irregular tooth surfaces feel different when you run your tongue across them. Healthy enamel is smooth. Cavities create rough edges and uneven textures. This tactile exploration can sometimes detect problems before they’re visible.
White spots around the edges of your teeth or near the gum line might indicate early enamel demineralization. These precavities appear as chalky white patches and represent your tooth’s first line of distress. Interestingly, detecting issues at this stage is similar to how you might learn to tell if a diamond is real—it requires careful observation of subtle surface changes.
Cavities between teeth are particularly sneaky because they’re invisible without special tools or X-rays. You might notice slight swelling of the gums between teeth or a persistent food trap where debris gets stuck repeatedly.
Physical Sensations and Pain Patterns
Your mouth is incredibly sensitive, and it communicates problems through distinct sensations. Understanding these signals helps you distinguish between normal tooth sensitivity and actual decay:
Sharp, localized pain when eating or drinking usually points toward a cavity rather than general sensitivity. This pain comes from stimulation reaching the nerve inside your tooth. Genuine sensitivity feels more like a dull ache, while cavity pain tends to be sharper and more specific to one tooth.
Lingering pain after eating is significant. With sensitivity, discomfort typically stops once you remove the trigger. Cavity pain often persists for several minutes or longer after the stimulus is gone. This prolonged response indicates nerve irritation from advancing decay.
Throbbing pain suggests infection or inflammation inside the tooth. This pulsating sensation, especially if it keeps you awake at night, indicates the cavity has likely reached the pulp chamber where the nerve lives. This stage requires immediate professional attention.
Pain when lying down happens because blood pressure increases in your head when horizontal, putting additional pressure on an inflamed tooth nerve. If your cavity pain worsens when you recline, it’s a sign the infection is progressing.

Temperature sensitivity deserves special mention. While some teeth naturally react to hot and cold, cavity-related sensitivity feels different. It’s more intense, more localized, and often accompanied by other symptoms on this list.
Risk Factors That Increase Cavity Likelihood
Not everyone develops cavities at the same rate. Certain factors significantly increase your risk, and understanding them helps you assess whether your symptoms warrant concern:
- Poor oral hygiene: Inconsistent brushing and flossing allows plaque to accumulate, feeding bacteria that create decay.
- High sugar consumption: Bacteria feast on dietary sugars, producing acids that attack enamel. Frequent snacking and sugary drinks create a constant feeding environment for these destructive bacteria.
- Acidic foods and beverages: Sodas, citrus juices, and wine directly weaken enamel. This weakening makes teeth more susceptible to cavities, similar to how moisture affects other materials you might assess—like determining if eggs are good based on their condition.
- Dry mouth: Saliva protects teeth by neutralizing acids and washing away food particles. Reduced saliva production significantly increases cavity risk.
- Existing dental work: Faulty fillings, crowns, or bridges create gaps where bacteria can hide and multiply.
- Age factors: Teenagers and older adults face elevated cavity risk due to dietary habits and receding gums respectively.
- Family history: Genetic factors influence cavity susceptibility. If your parents had frequent cavities, you’re more likely to develop them too.
Identifying which risk factors apply to you helps explain why cavities might be forming and guides your prevention strategy going forward.
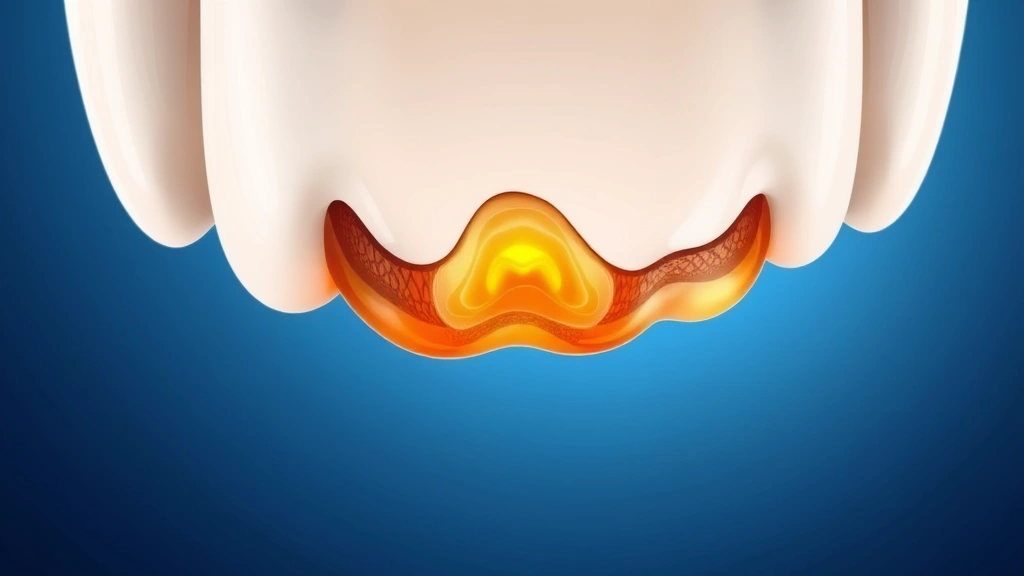
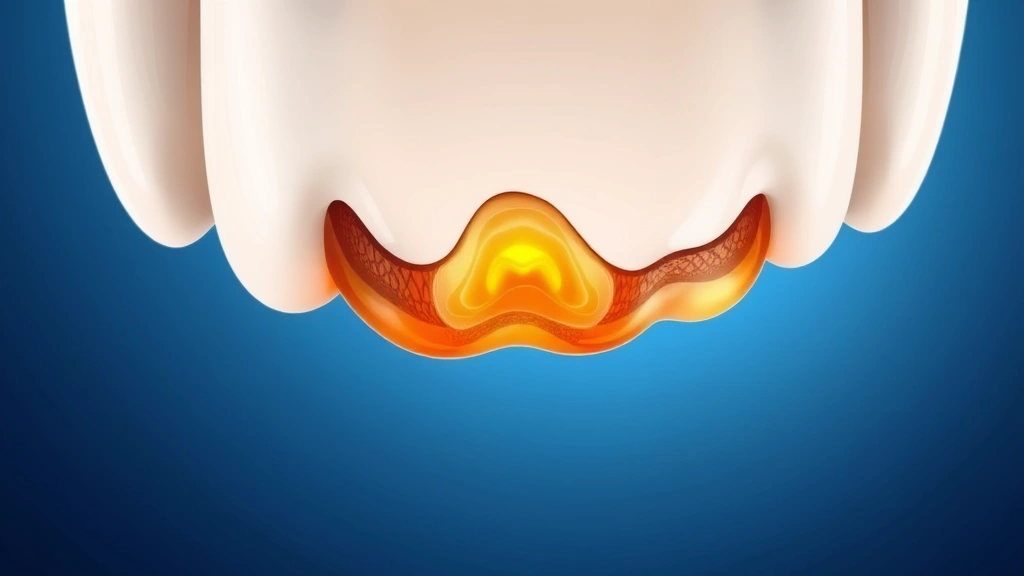
Understanding Cavity Stages
Cavities don’t appear fully formed overnight. They develop in stages, and recognizing which stage you’re in determines urgency and treatment options:
Stage 1: Enamel Decay starts when bacteria produce acids that attack the hard outer enamel layer. At this stage, you might see white spots but likely experience no pain. The decay is still superficial and potentially reversible with aggressive fluoride treatment. This early detection is crucial because intervention at this point can stop progression entirely.
Stage 2: Enamel Breakdown occurs when decay penetrates through the enamel layer. You’ll likely notice discoloration becoming darker and more defined. Sensitivity might begin as the underlying dentin layer becomes exposed. Reversing decay at this stage is unlikely, but professional treatment can still prevent further progression.
Stage 3: Dentin Decay develops when decay reaches the softer layer beneath enamel. This stage brings noticeable sensitivity and pain because dentin contains tubules leading directly to the nerve. Decay spreads faster through dentin than enamel, so intervention becomes increasingly urgent.
Stage 4: Pulp Involvement represents advanced decay that has reached the innermost pulp chamber containing the nerve and blood vessels. This stage causes significant pain, potential infection, and may require root canal treatment rather than a simple filling. The decay might also affect the jawbone if left untreated.
Each stage progression typically takes months or years, depending on your oral hygiene and dietary habits. This timeline emphasizes why regular dental checkups matter—your dentist can catch decay at earlier stages before you feel symptoms.
Prevention: The Best Detection Method
Here’s the truth nobody wants to hear but everyone needs to understand: preventing cavities is infinitely easier than treating them. While this guide focuses on detection, prevention deserves equal attention because the best cavity you’ll ever have is one that never forms.
Brush twice daily with fluoride toothpaste for two minutes each time. This simple habit removes plaque before it hardens and protects enamel with fluoride. Most people brush for only sixty seconds, which isn’t enough time to thoroughly clean all surfaces.
Floss daily to remove food and plaque from between teeth where your toothbrush can’t reach. This is where approximately 40% of tooth surfaces live, making flossing non-negotiable for cavity prevention. Think of it as being thorough in your assessment—much like you’d carefully evaluate if a watermelon is ripe by checking all indicators rather than just one.
Limit sugary foods and drinks. Bacteria don’t need much—even small amounts of sugar trigger acid production. Reducing frequency of consumption matters more than quantity. One soda with a meal is better than sipping it throughout the day.
Drink water instead of acidic beverages. Water rinses your mouth naturally and contains no sugars or acids. If you do consume acidic drinks, use a straw to minimize contact with teeth and rinse with water afterward.
Use fluoride mouthwash as an additional protective layer. This isn’t a replacement for brushing and flossing, but it provides extra reinforcement.
Visit your dentist every six months for professional cleanings and examinations. Professional cleanups remove tartar that home care can’t address, and X-rays detect decay before you notice symptoms.
Consider dental sealants if you have deep grooves in your molars. These plastic coatings fill the crevices where decay commonly starts, providing targeted protection for high-risk areas.
When to Seek Professional Help
Self-diagnosis has limits. While recognizing cavity symptoms is valuable, professional evaluation is essential for confirmation and treatment. Here’s when you absolutely should schedule an appointment:
Immediate scheduling: Contact your dentist if you experience severe pain, visible holes in teeth, signs of infection (swelling, pus, fever), or pain that interferes with eating or sleeping. These indicate advanced decay requiring prompt treatment.
Within a week: Book an appointment if you notice persistent sensitivity localized to one tooth, visible discoloration you haven’t seen before, or any combination of symptoms from this guide. Early intervention prevents progression.
Routine visit: If you’re simply noticing subtle changes or want professional confirmation, your regular six-month checkup is appropriate timing.
Professional detection methods your dentist uses include visual examination, X-rays (which reveal decay between teeth and below the gum line), and laser fluorescence technology that detects early enamel demineralization. These tools catch cavities far earlier than you can at home.
According to the American Dental Association, approximately 92% of adults have experienced cavities in permanent teeth. You’re not alone in this struggle, and professional dentists handle cavity detection and treatment every single day.
Treatment options depend on cavity stage. Early-stage decay might reverse with fluoride treatment. Established cavities require fillings. Advanced decay with pulp involvement needs root canal therapy. Your dentist will explain options specific to your situation and help you choose the best approach.
For comprehensive information about cavity causes and prevention, Mayo Clinic provides detailed medical guidance that complements this practical detection guide.
Frequently Asked Questions
How quickly do cavities develop?
Cavity development varies based on individual factors, but the process typically takes months to years. Early-stage enamel decay might progress slowly, while advanced decay in dentin spreads faster. Aggressive acid environments (high sugar consumption, frequent acidic beverages) accelerate the timeline. Regular dental visits catch decay before it becomes painful or requires extensive treatment.
Can you feel a cavity with your tongue?
Sometimes, yes. You might detect rough spots, pits, or unusual textures when running your tongue across teeth. However, many early cavities feel smooth and aren’t detectable this way. Visual inspection and professional examination are more reliable than tactile exploration alone. This sensory approach is somewhat like how you might assess whether pearls are real—touch and appearance combine for better evaluation.
Do all cavities cause pain?
No. Early-stage cavities confined to enamel typically cause no pain. Many cavities don’t hurt until they’ve progressed significantly. This is why you can’t rely solely on pain as a detection signal. Regular dental checkups are essential because they find cavities before symptoms develop.
What’s the difference between a cavity and a stain?
Stains are surface discoloration that don’t involve structural damage. They might be brown or dark but feel smooth. Cavities create pits, holes, or rough spots and typically involve deeper discoloration. Stains respond to whitening or professional cleaning, while cavities require filling. Your dentist can distinguish between them instantly.
Can cavities be reversed?
Very early-stage cavities confined to enamel with white spot demineralization can sometimes be reversed through aggressive fluoride treatment and improved oral hygiene. Once decay has progressed to visible brown or black spots or created structural damage, reversal isn’t possible—only treatment through filling or more extensive procedures. This emphasizes why early detection matters so much.
Are back teeth more prone to cavities?
Yes. Molars and premolars have deep grooves and are harder to clean thoroughly. Food particles hide in these crevices, and flossing these areas requires careful technique. Back teeth also bear more chewing force, which can stress enamel. Dental sealants specifically target these high-risk areas. This susceptibility is similar to how certain conditions are more likely to occur—just as you’d check if eggs are bad more carefully under certain circumstances, back teeth deserve extra attention.
Does cavity pain come and go?
Yes, cavity pain is often intermittent, especially in early stages. It might flare up when eating sugary foods, drinking hot or cold beverages, or when pressure is applied. As decay advances and involves the nerve, pain becomes more constant. The pattern of pain—intermittent versus constant—can indicate cavity progression stage.
How accurate are at-home cavity detection methods?
At-home detection catches obvious cavities but misses early-stage decay and cavities between teeth. Professional tools like X-rays and specialized light detection are far more accurate. Think of at-home detection as a preliminary screening, not a definitive diagnosis. Professional confirmation is always necessary for treatment decisions.
What should I do if I suspect a cavity but can’t see a dentist immediately?
While you wait for your appointment, avoid chewing on the affected side, rinse with salt water to reduce inflammation, use over-the-counter pain relievers as directed, and avoid very hot, cold, or hard foods. These measures provide temporary relief but don’t treat the underlying decay. Don’t delay scheduling—the longer you wait, the more the cavity progresses and the more expensive treatment becomes.



