
How Long for Dissolvable Stitches to Dissolve? A Complete Timeline Guide
If you’ve recently had surgery, a wound closure, or a medical procedure, you might be wondering about that timeline for dissolvable stitches. Unlike traditional stitches that require removal, absorbable sutures are designed to break down naturally over time. But here’s the thing—the dissolution process isn’t one-size-fits-all, and understanding what to expect can help you manage your recovery with confidence and peace of mind.
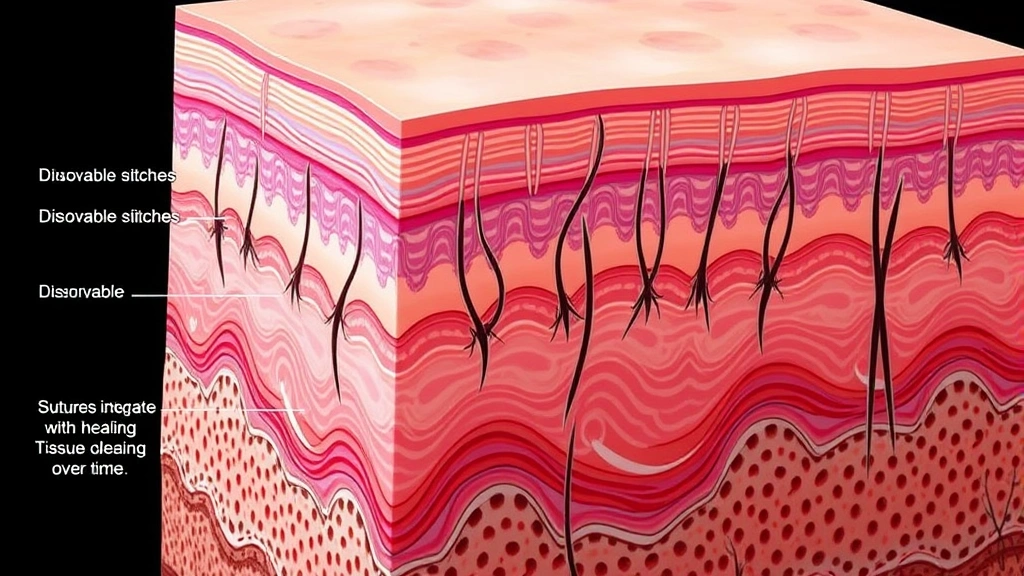
Dissolvable stitches, also known as absorbable sutures, are made from materials that your body gradually breaks down and absorbs. They’re commonly used in surgical procedures, wound closures, and various medical treatments because they eliminate the need for a follow-up appointment to have them removed. However, the timeline for complete dissolution varies significantly depending on the type of suture material, the location of the wound, and individual healing factors.
In this comprehensive guide, we’ll explore everything you need to know about dissolvable stitches—from how long they actually take to dissolve to what you should do if something seems off during the healing process.
Timeline for Dissolvable Stitches Dissolution
The dissolution timeline for absorbable stitches typically ranges from five days to three weeks, though some specialized sutures can take significantly longer. Most commonly, you’ll see the majority of dissolution occur within the first two weeks following your procedure.
For minor wounds and superficial cuts, dissolvable stitches often break down within five to seven days. These are usually placed on areas like the face, scalp, or other highly visible locations where quick healing is desired. The body’s natural inflammatory response and enzymatic activity work efficiently on these surface-level stitches.
For deeper wounds or surgical incisions, the timeline extends considerably. Stitches placed in muscle tissue, organs, or deep layers of skin can take anywhere from two to four weeks to fully dissolve. This extended timeline allows the deeper tissues adequate time to heal and gain strength before the sutures are completely absorbed.
Some specialized absorbable sutures, particularly those used in orthopedic surgery or complex internal procedures, can remain intact for six to eight weeks or longer. Your surgeon will specify which type was used and provide an estimated dissolution timeline during your post-operative instructions.
Factors Affecting Dissolution Speed
Several variables influence how quickly your dissolvable stitches will break down. Understanding these factors helps you set realistic expectations for your recovery journey.
Wound Location and Depth plays a crucial role. Stitches in areas with higher blood flow dissolve faster because increased circulation delivers more enzymes and immune cells to the wound site. Conversely, areas with limited blood supply—like certain parts of the legs or feet—experience slower dissolution. Similarly, deeper wounds require longer-lasting sutures to maintain wound integrity during the critical healing phases.
Your Body’s Healing Capacity varies based on age, overall health, and metabolic rate. Younger individuals typically experience faster suture dissolution due to more robust immune function and faster cellular turnover. Those with compromised immune systems, diabetes, or poor circulation may experience delayed dissolution.
Infection Status dramatically affects the timeline. If your wound becomes infected, the inflammatory response intensifies, which can actually speed up suture breakdown—but this isn’t necessarily beneficial since it happens before the wound is adequately healed. This is why infection prevention is critical.
Suture Tension and Placement matter significantly. Stitches under greater tension or placed in areas with constant movement dissolve more slowly because your body needs them longer to maintain structural integrity. Areas prone to stretching or flexing require more durable sutures.
Environmental Factors including moisture, temperature, and UV exposure can influence dissolution rates. Wounds kept in moist environments (like those covered with bandages) may dissolve slightly faster than exposed wounds, though this depends on the specific suture material.
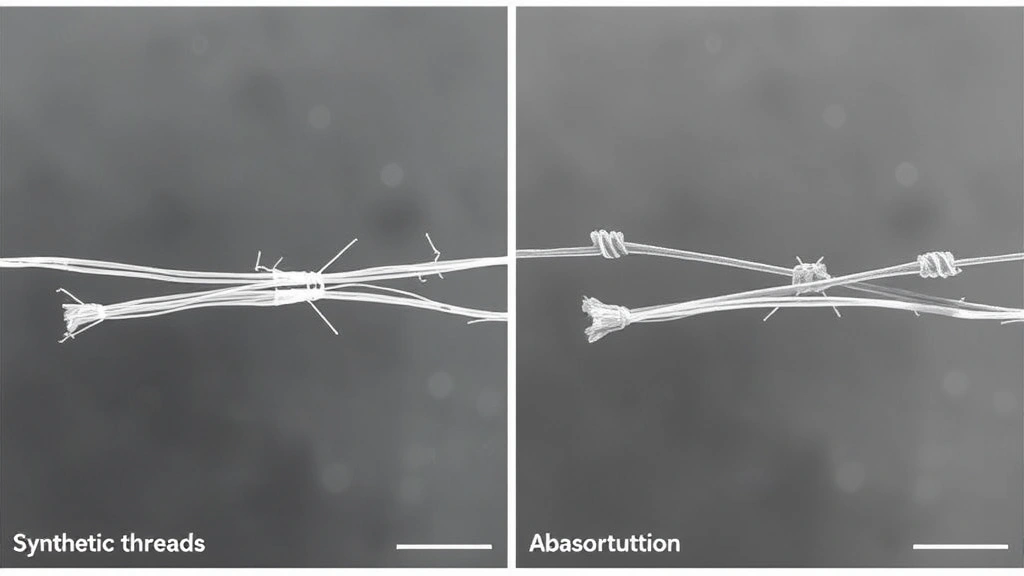
Types of Absorbable Suture Materials
Different suture materials dissolve at different rates, and your healthcare provider selects the appropriate type based on your specific procedure and wound characteristics.
Plain Gut Sutures are among the oldest absorbable materials and dissolve relatively quickly—typically within five to seven days. They’re derived from animal intestines and are rarely used today due to inconsistent dissolution rates and higher infection risk. However, you might encounter them in certain specialty procedures.
Chromic Gut Sutures are treated chemically to slow dissolution, lasting approximately two to three weeks. They’re more predictable than plain gut sutures and resist enzymatic breakdown better, making them suitable for slightly deeper wounds that need moderate-term support.
Polyglycolic Acid (PGA) sutures dissolve within two to four weeks and maintain approximately 75% of their strength for the first two weeks. They’re synthetic, predictable, and commonly used in general surgery and gynecological procedures.
Polylactic Acid (PLA) sutures provide longer-term support, typically dissolving over six to twelve months. These are ideal for procedures requiring extended wound support, such as joint repair or complex surgical reconstructions.
Polydioxanone (PDO) sutures offer excellent strength retention and dissolve gradually over four to six weeks. They’re particularly popular in cosmetic surgery because they maintain tension during the critical healing window while remaining strong enough to prevent wound dehiscence.
Polyglactin 910 sutures combine predictability with moderate dissolution time—typically two to three weeks—making them versatile for various surgical applications. They’re among the most commonly used absorbable sutures in modern medicine.
Understanding the specific material your healthcare provider used helps you anticipate the dissolution timeline. If you’re unsure which type was used, don’t hesitate to ask your surgeon or check your discharge paperwork.
Proper Wound Care During Healing
While your dissolvable stitches work their magic, you play an active role in supporting the healing process and ensuring optimal outcomes.
Keep the Wound Clean by gently washing it with mild soap and lukewarm water. Pat it dry carefully with a clean cloth—never rub. If your healthcare provider recommends specific wound cleansing solutions, follow those instructions precisely. Clean wounds heal faster and with fewer complications.
Maintain Proper Moisture Balance by keeping the wound covered if it’s in an area prone to contamination, but allow it to breathe when possible. Most modern wound care emphasizes moist healing environments, which promote faster tissue regeneration. Your surgeon will provide specific dressing recommendations.
Avoid Submerging the wound in water (like bathing or swimming) for the duration recommended by your healthcare provider—typically until the stitches are partially or fully dissolved. Excessive moisture can soften the sutures prematurely and compromise wound integrity.
Protect from Friction and Tension by wearing appropriate clothing that won’t rub against the wound site. If your stitches are on a joint or area subject to movement, consider limiting that movement during the early healing phase. Some wounds benefit from protective bandaging or specialized wound covers.
Watch for Signs of Infection including increased redness, warmth, swelling, pus, or foul odor. A little inflammation is normal, but excessive symptoms warrant immediate medical attention. Similarly, if you notice the wound opening up or stitches breaking prematurely, contact your healthcare provider promptly.
If you’re dealing with other healing situations, understanding timelines helps with planning. For instance, if you’re also managing a recovery from hemorrhoids, coordinating multiple healing processes requires careful wound management. Just as managing belly button piercing healing requires patience and proper care, surgical recovery demands consistent attention to your wound.
Avoid Strenuous Activity during the critical early healing phase. Your surgeon will provide specific guidelines, but generally, heavy lifting, intense exercise, or activities that increase blood pressure should be limited until the wound shows significant healing progress.
When to Worry: Complications and Warning Signs
While dissolvable stitches are generally safe and effective, complications can occasionally arise. Knowing what to watch for helps you seek timely medical intervention if needed.
Infection Symptoms are your primary concern. Signs include increasing pain (beyond initial discomfort), redness spreading outward from the incision, warmth to the touch, pus or discharge with foul odor, fever, or red streaking extending from the wound. These symptoms require immediate medical attention—don’t wait to see if they resolve on their own.
Allergic Reactions to suture material, though rare, can occur. You might notice unusual itching, hives, or localized swelling around the stitches. If you have a known history of material sensitivities, inform your healthcare provider before the procedure.
Premature Suture Dissolution can happen if stitches break or dissolve before the wound is adequately healed. Signs include the wound reopening, visible separation of incision edges, or stitches disappearing much faster than expected. Contact your surgeon immediately if you notice this.
Delayed Dissolution is less urgent but still worth monitoring. If stitches remain intact significantly longer than expected (beyond the anticipated timeline by several weeks), your surgeon may want to evaluate them. Sometimes sutures become encapsulated by tissue and require professional removal.
Granulation Tissue Formation can occur around stitches, creating small red bumps. This is usually normal as your body heals, but excessive granulation tissue might warrant evaluation.
Keloid or Hypertrophic Scar Formation is more common in certain individuals and skin types. If you notice excessive scarring developing, discuss treatment options with your healthcare provider. Understanding your skin’s healing tendencies—similar to how tattoo healing varies by individual—helps you anticipate potential complications.
Just as you might research nose piercing healing timelines before getting pierced, understanding potential surgical complications before your procedure allows you to recognize warning signs early.
Suture Abscess occasionally develops if your body reacts to the suture material. You might notice a small, localized bump or drainage around a specific stitch. This usually resolves as the suture dissolves, but inform your healthcare provider if you’re concerned.
Frequently Asked Questions
Can I shower or bathe with dissolvable stitches?
Generally, yes—but with precautions. Light showers are usually fine after the first 24-48 hours, though you should avoid prolonged water exposure or full submersion in bathtubs. Keep the wound as dry as possible and pat it dry gently afterward. Your surgeon will provide specific guidelines based on your particular procedure and wound location.
What should I do if a dissolvable stitch falls out early?
Contact your healthcare provider promptly. If it’s very early in the healing process, the wound might not be strong enough without all stitches intact. Your provider may recommend protective bandaging, limiting activity, or scheduling an evaluation to assess wound integrity.
Is it normal for dissolvable stitches to itch?
Some itching is normal as your body heals, but excessive itching could indicate infection, allergic reaction, or skin irritation. Resist the urge to scratch, as this can introduce bacteria or damage the healing wound. If itching is severe or persistent, contact your healthcare provider.
How do I know if my stitches are dissolving properly?
Gradual dissolution is usually subtle. You might notice the stitches becoming slightly less prominent, fraying at the ends, or becoming looser over time. The wound should gradually close and heal around the dissolving sutures. If you’re unsure whether dissolution is progressing normally, ask your healthcare provider during a follow-up visit.
What if my dissolvable stitches don’t dissolve after the expected timeline?
This occasionally happens, particularly with deeper stitches or in individuals with certain healing characteristics. Your body might encapsulate the sutures, preventing complete dissolution. Contact your healthcare provider if stitches remain after the expected timeline plus a reasonable buffer (usually 2-4 additional weeks). Your surgeon may need to remove them manually.
Can I exercise or play sports with dissolvable stitches in place?
This depends on the location and depth of your stitches, plus the intensity of the activity. Generally, light activities are fine, but strenuous exercise, heavy lifting, or contact sports should be avoided until your surgeon gives clearance. Activities that increase blood pressure or create tension on the wound can compromise healing and cause premature suture dissolution or wound reopening.
Are dissolvable stitches stronger than regular stitches?
Strength depends on the specific material, not whether stitches are dissolvable or not. Modern absorbable sutures are engineered to maintain adequate strength throughout the critical healing period. Your surgeon selects the appropriate material based on the strength requirements of your specific wound.
Will dissolvable stitches leave scars?
Scarring depends on numerous factors including wound depth, location, individual healing response, and post-operative care—not specifically on whether stitches are dissolvable or not. Proper wound care and sun protection during healing can minimize scar appearance. Much like understanding timelines for removing adhesive substances from skin, scar management requires proper technique and patience.
How long should I wait before returning to normal activities?
This varies significantly based on the procedure, wound location, and your overall health. Minor procedures might allow normal activity within a few days, while more extensive surgery might require several weeks of modified activity. Your healthcare provider will give you specific restrictions and clearance timelines.
What’s the difference between dissolvable and non-dissolvable stitches?
The primary difference is that dissolvable stitches break down naturally over time, eliminating the need for removal, while non-dissolvable stitches require manual removal at a follow-up appointment. Dissolvable stitches are more convenient but can’t be removed if complications arise. Your surgeon chooses based on the wound characteristics and desired healing timeline.
